Cancer cell lines
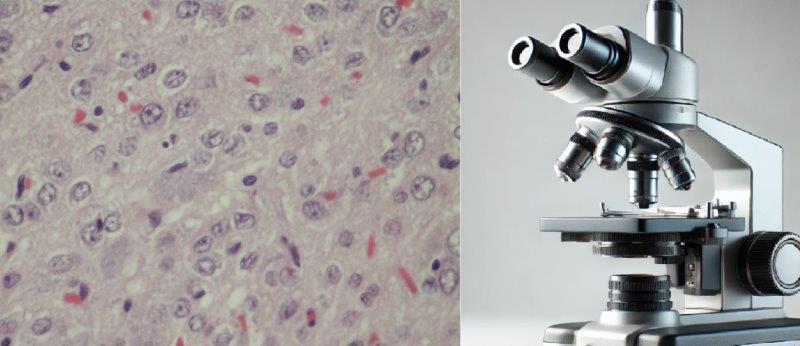
Cancer cell lines are populations of cancer cells that have been adapted to grow continuously in culture. These cells are derived from human or animal tumors and are grown under controlled laboratory conditions to study cancer biology, drug development, and therapeutic responses. Cancer cell lines originate from primary tumor tissues or metastatic sites of patients with cancer. The tissue is processed and the cancer cells are isolated and cultured. Over time, these cells acquire the ability to proliferate indefinitely, making them immortal in a laboratory setting. In 1951, the first cancer cell lines were developed from human cervical tumors. These HeLa cells started to propagate in the artificial environment. Other famous examples include: MCF-7, a breast cancer cell line and A549, a lung cancer cell line.
Cancer cell lines share many characteristics of the original tumor, but there are also differences due to mutations and adaptations that occur during culturing. There are several important features of cancer cell lines, including the uncontrolled growth – these cells continue dividing beyond normal regulatory controls. Also, genetic instability – over time, they can accumulate additional mutations. Ability to survive in culture – these cells adapt to in vitro conditions with specific nutrient requirements and environmental factors like temperature and pH. And finally – variation across lines – each cell line has distinct genetic, epigenetic, and biochemical profiles that reflect the tumor of origin.
Cancer cell lines are essential tools for understanding cancer and developing treatments. They are widely used for drug screening and discovery, testing the effects of new compounds on cancer cell proliferation, survival, and apoptosis. Genetic and molecular studies to discover cancer-associated genes, mutations, signaling pathways, and protein expressions. Tumor biology for investigating mechanisms such as metastasis, invasion, angiogenesis, and tumor microenvironment interactions. Finally, to be utilized in personalized medicine some cell lines are derived from patient-specific tumors and help test treatments tailored to genetic profiles. However, there are certain disadvantages – while cancer cell lines are widely used, they have some limitations including genetic drift – over long periods in culture, cell lines can diverge from the original tumor due to genetic mutations. Also, lack of tumor microenvironment within in vitro models lack the complex interactions present in a living organism, including immune responses, stromal cells, and blood supply. Finally, cell lines represent a uniform population of cancer cells (clonal populations), which doesn’t fully reflect the heterogeneity seen in tumors in patients. Additionally, some cell lines are prone to contamination with other cell types, leading to inaccurate results.
With advances in cancer research, the use of patient-derived xenografts (PDX) and organoids have emerged as alternatives or complements to traditional cancer cell lines. List of validated xenograft models commercially availble from Altogen Labs – altogenlabs.com/xenograft-models. These models better replicate the tumor architecture and the genetic diversity of cancers. In conclusion, cancer cell lines are invaluable tools in oncology research, allowing scientists to dissect cancer mechanisms and develop potential therapies. However, they should be used with awareness of their limitations and supplemented with other models for comprehensive research.
Different cancer cell lines
Cancer cell lines are an essential tool in cancer research, allowing scientists to study cancer biology, drug responses, and genetic mutations in a controlled laboratory setting. These cell lines are derived from various human tumors and are grown under specific conditions to simulate the in vivo environment of the original cancer cells. By using cancer cell lines, researchers can observe how cancer cells behave, test potential drugs, and explore the mechanisms behind cancer progression. At the end of 1980, a project began known as the “National Cancer Institute 60 (NCI-60) anticancer drug discovery.” This initiative screened numerous pharmacological compounds to assess their anticancer activity. The project originally introduced cell lines representing nine human cancer types: breast, kidney, CNS, leukemia, colon, ovary, lung, prostate, and melanoma.
There are numerous cancer cell lines representing different types of human cancers. Examples:
Breast Cancer Cell Lines: MCF-7 and T-47D. These cell lines are used to study breast cancer’s behavior, response to hormones like estrogen, and potential treatments.
Lung Cancer Cell Lines: A549 is a common cell line used to investigate non-small cell lung cancer (NSCLC), helping researchers understand lung cancer progression and drug sensitivity.
Colon Cancer Cell Lines: HT-29 and HCT116 are widely used to explore the mechanisms behind colon cancer and test chemotherapy drugs.
Leukemia Cell Lines: K562 and HL-60 cell lines are derived from blood cancers and are utilized to study leukemia’s biological properties and responses to treatment.
Melanoma Cell Lines: SK-MEL-28 and A375 are used for studying skin cancer, particularly how melanoma cells evade immune responses and their resistance to therapies.
The NCI-60 panel, a collection of 60 cancer cell lines representing nine different types of human cancers: breast, kidney, central nervous system (CNS), leukemia, colon, ovary, lung, prostate, and melanoma. This panel was created by the National Cancer Institute (NCI) and has played a pivotal role in drug screening, helping researchers identify potential anticancer compounds and their mechanisms of action.
CULTURING AND Establishment of Cancer Cell Lines
Culturing cancer cells in vitro involves isolating them from the original tumor and growing them in controlled conditions. Researchers provide essential nutrients and factors, such as mitogenic and co-mitogenic agents, to maintain the growth, viability, and characteristics of the cancer cells. These agents help initiate cell division and prevent apoptosis (programmed cell death), ensuring that the cancer cells proliferate and behave similarly to how they would in the body.
In an in vitro environment, cancer cells are isolated from tumors and cultured under controlled conditions to create cancer cell lines. Proper isolation techniques and the provision of specific supplements are essential to support the growth and survival of these cells. To mimic the in vivo environment, researchers introduce mitogenic and co-mitogenic agents, which stimulate cell division and prevent programmed cell death, or apoptosis. These agents help maintain the cancer cells’ viability, genotype, and phenotype in the laboratory setting, allowing them to behave similarly to how they would in a living organism. The first step in creating a cancer cell line involves isolating cancer cells from a patient’s tumor or metastatic site. This can be done through surgical biopsy, followed by careful extraction of the tumor cells. Once isolated, the cells are placed in a culture medium containing the necessary nutrients, growth factors, and supplements that support their continued proliferation. These include essential amino acids, vitamins, and growth factors that mimic the natural environment of cancer cells. To ensure the continuous growth of cancer cells, mitogenic agents (which promote cell division) and co-mitogenic agents (which enhance the effects of mitogens) are introduced. These factors are critical for the early stages of cell line establishment and help to prevent the cells from undergoing apoptosis. As the cancer cells begin to grow, clonal propagation occurs. This means that individual cancer cells divide and form colonies, resulting in a population of cells that are genetically identical to the original cancer cell. This process is vital for creating stable, reproducible cell lines that can be used for consistent research. Once established, the cancer cell line can be maintained over time, allowing researchers to study cancer behavior, test potential therapies, and explore genetic mutations. These cell lines can be frozen and revived, ensuring a long-term, renewable source of cancer cells for study.
The establishment of cancer cell lines is a fundamental process in cancer research. By isolating and cultivating tumor cells under controlled conditions, researchers can create reliable models for studying cancer mechanisms and developing therapies. With ongoing advancements in cell culture techniques, these models continue to evolve, providing critical insights into cancer biology and treatment.
The Clinical Significance of Cancer Cell Lines
Cancer cell lines play a pivotal role in clinical research, serving as vital tools for understanding cancer biology and developing therapeutic interventions. These cell lines, derived from human tumors, provide a controlled environment for studying the molecular mechanisms underlying cancer progression, genetic mutations, and tumor behavior. Their clinical significance lies in their use for drug screening, where potential anticancer compounds can be tested for efficacy and toxicity before advancing to clinical trials.
Additionally, cancer cell lines allow for the exploration of personalized medicine by examining how specific genetic profiles respond to targeted therapies. By offering insights into tumor growth, metastasis, and resistance to treatment, cancer cell lines contribute to the development of more effective and individualized cancer treatments, ultimately improving patient outcomes. Despite some limitations, such as the lack of a complete tumor microenvironment, cancer cell lines remain invaluable in bridging the gap between basic cancer research and clinical applications.
Cancer cell lines are used to screen potential therapeutic compounds to assess their ability to kill cancer cells or inhibit their growth. Researchers study the genetic makeup of cancer cells to identify mutations and understand the molecular drivers of cancer. Cell lines allow scientists to explore fundamental cancer processes, such as metastasis, angiogenesis, and resistance to therapy. Despite their extensive use, cancer cell lines have limitations. They can accumulate genetic changes over time, diverging from the original tumor’s characteristics. Additionally, since they are cultured outside the body, they lack the complex tumor microenvironment, including immune system interactions and surrounding tissue, which plays a critical role in cancer progression. Cancer cell lines remain a cornerstone of cancer research, offering a controlled environment for studying various types of cancer. While they have some limitations, they have been instrumental in improving our understanding of cancer and developing new treatments.
Cancer Cell Lines AND TRANSFECTION
Cell line transfection reagents are specialized chemical or biological agents used to introduce nucleic acids, such as DNA, RNA, or siRNA, into cells. These reagents facilitate the delivery of genetic material across the cell membrane, enabling researchers to manipulate gene expression for various applications, including gene knockdown, overexpression, and genome editing. Transfection reagents are tailored to the specific requirements of different cell lines, optimizing efficiency and minimizing cytotoxicity. They are essential tools in molecular biology and biomedical research, widely used in cancer studies, drug discovery, and gene therapy development.
Transfection kits must be designed and optimized to deliver the cargo biomolecules with high efficiency and low cytotoxicity in different cancer cell lines. Altogen Biosystems is a leading manufacturer of formulated transfection reagents to meet the unique characteristics of specific cell lines, ensuring effective delivery of nucleic acids, such as DNA, RNA, and siRNA, into target cells.
Examples of some of the specialized transfection kits for common cancer cell lines:
MCF-7 Transfection Kit (Breast Cancer Cell Line) The MCF-7 cell line, derived from human breast cancer, is widely used in hormone-responsive cancer research. This MCF-7 Transfection Kit is optimized for high transfection efficiency in this cell line, providing reliable results in gene expression studies and RNA interference experiments with minimal cytotoxicity.
A549 Transfection Kit (Lung Cancer Cell Line) A549 is a non-small cell lung cancer (NSCLC) cell line, commonly used in lung cancer research. The A549 Transfection Kit is specifically designed to efficiently transfect this line, facilitating studies in gene function, drug resistance, and cancer cell biology.
HT-29 Transfection Kit (Colon Cancer Cell Line) The HT-29 colon cancer cell line is important for colorectal cancer research, including studies on chemotherapy resistance. HT-29 Transfection Kit delivers high transfection efficiency, ensuring effective gene knockdown or overexpression, making it suitable for drug screening and genetic analysis.
PC-3 Transfection Kit (Prostate Cancer Cell Line) The PC-3 cell line is a well-established model for studying prostate cancer, especially in androgen-independent contexts. PC-3 Transfection Kit provides reliable results in gene expression and silencing studies, helping to advance research into prostate cancer progression and therapeutic targets.
U87 Transfection Kit (Glioblastoma Cell Line) U87 cells are derived from human glioblastoma and are widely used in brain cancer research. The U87 Transfection Kit is designed for optimal transfection of this difficult-to-transfect cell line, facilitating studies on brain tumor biology and therapeutic approaches.
IN VIVO TRANSFECTION REAGENTS IN CANCER RESEARCH
In vivo transfection reagents are specialized formulations used to deliver nucleic acids (such as plasmid DNA, siRNA, miRNA, or mRNA) directly into living organisms, bypassing the barriers of cellular membranes to introduce genetic material into target tissues or organs. These reagents are designed to ensure stability, protect nucleic acids from degradation, and facilitate efficient gene delivery in a physiological environment. In cancer research, in vivo transfection is crucial for studying gene function, exploring the molecular mechanisms driving tumor development, and testing the efficacy of gene-based therapies in animal models. By enabling researchers to manipulate gene expression within a living system, in vivo transfection reagents help in evaluating therapeutic potential, studying tumor microenvironment interactions, and advancing personalized treatment approaches.
Examples of tissue-targeted in vivo transfection kits optimized for efficient gene delivery in animal models:
Lung In Vivo Transfection Kit This reagent is specifically optimized for delivering nucleic acids to lung tissue. It provides efficient and localized transfection, allowing researchers to study lung-specific gene expression, lung cancer therapies, and respiratory diseases in animal models.
Liver In Vivo Transfection Kit The Liver In Vivo Transfection Kit is formulated for efficient gene delivery to liver tissue, which is critical for studying liver cancer, metabolic disorders, and liver-specific gene therapies. This reagent ensures high transfection efficiency with minimal immune response in animal models.
Kidney In Vivo Transfection Kit Designed for kidney-targeted gene delivery, this kit is ideal for researching renal diseases and cancers. The Kidney In Vivo Transfection Kit allows for effective gene silencing and overexpression in kidney tissues, enabling in vivo studies of renal cancer and therapeutic development.
Pancreas In Vivo Transfection Kit The Pancreas In Vivo Transfection Kit is tailored for delivering genetic material to the pancreas. It is suitable for studies on pancreatic cancer, diabetes, and other pancreatic diseases, providing high transfection efficiency with localized delivery to the pancreas.
Brain In Vivo Transfection Kit This kit is designed for gene delivery to the central nervous system, particularly the brain. The Brain In Vivo Transfection Kit is used in neurological research, including studies on brain tumors, neurodegenerative diseases, and gene therapy applications targeting the brain.
These tissue-targeted in vivo transfection kits are designed to provide reliable and reproducible results for various applications, including gene silencing, gene overexpression, and therapeutic testing in cancer research. Transfection reagents are used to test gene therapies that can either suppress oncogenes or promote tumor suppressor genes in animal models. Researchers use in vivo transfection to introduce genes or silencing RNA into tumors to study their effects on tumor growth, metastasis, and drug resistance. In vivo gene delivery enables the testing of potential gene-based drugs in preclinical models of cancer, helping evaluate their efficacy and safety. By manipulating gene expression in specific tissues, in vivo transfection contributes to the development of personalized therapies based on individual genetic profiles. A range of in vivo transfection kits provides reliable tools for researchers to study gene functions, test new cancer therapies, and explore the molecular mechanisms of diseases in living organisms, advancing both cancer research and therapeutic development.